Community-acquired pneumonia (CAP) is common and a leading cause of death worldwide.
Read the source article for this feature from
Critical Care Explorations.
Pneumonia causes about 6000 deaths per day globally and is the most common cause of death in children younger than 5 years,
1 according to James A. Russell, MD, a professor in the Division of Critical Care Medicine at University of British Columbia (UBC) and an investigator in the UBC Life Sciences Institute.
Many patients with CAP respond well to antibiotics, oxygen, and supplemental care.
2 However, some patients can deteriorate quickly with little warning, needing urgent resuscitation and ICU admission, where they may receive mechanical ventilation, vasopressor therapy, and renal replacement therapy (RRT).
A team of researchers developed several machine learning models to compare the models’ predictions with clinicians’ predictions. The findings were published in the June 2025 issue of
Critical Care Explorations.
3 “Machine learning has been really helpful in healthcare,” said first author George Chen, MD, a first-year internal medicine resident at UBC. “These computer science techniques are really good at combing through large datasets and finding complex patterns that we otherwise wouldn’t be able to immediately pick up with our own eyes.” There are so much data in patients’ electronic health records just waiting to be explored, he said.
The Findings
Dr. Chen teamed up with Dr. Russell, his mentor and the principal investigator of Community-Acquired Pneumonia: Toward InnoVAtive Treatment (CAPTIVATE). The researchers conducted a retrospective observational study of patients older than 18 years who were hospitalized without the need for invasive ventilation, vasopressors, and RRT on the day of admission. Subjects comprised 2420 patients with CAP and COVID-19 and 1909 patients with CAP but without COVID-19.
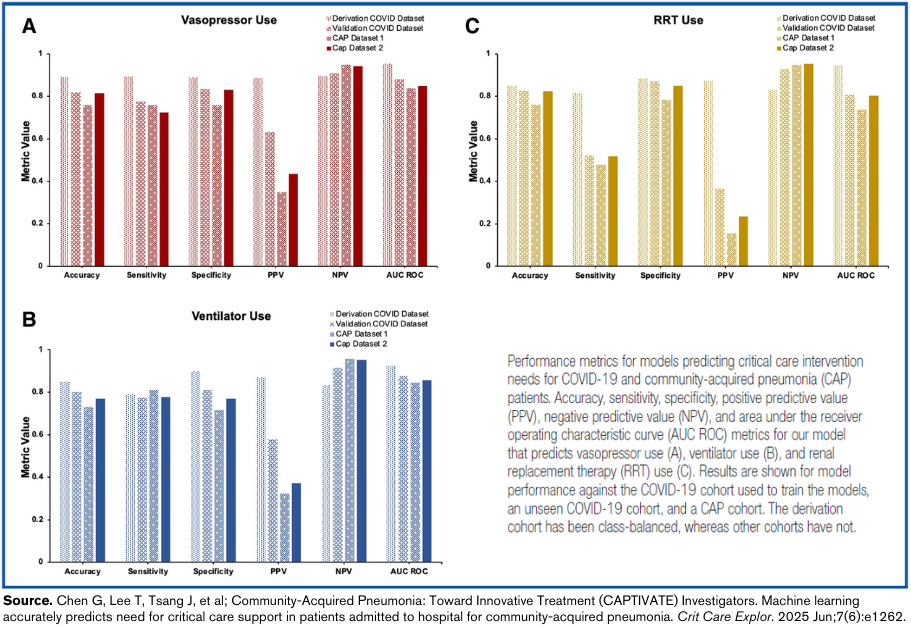
Of the several models they trained, models based on random-forest classifier (RFC) were most accurate. RFC was then used to predict three end points: eventual use of invasive ventilation, vasopressors, and RRT during hospitalization. The results were then validated in one COVID-19 CAP and two non-COVID-19 CAP cohorts.
The machine learning models were compared with logistic regression models. The RFC models were about 90% accurate in predicting the later need for more extreme interventions, while the logistic regression models were about 80% accurate. “Overall, we found that the machine learning algorithm was quite accurate in predicting whether or not a patient would eventually need critical care interventions—specifically vasopressor use, ventilator use, and RRT use—and that was just by looking at the day-of-admission variables,” Dr. Chen said.
Dr. Russell said that, because the study was conducted in 16 sites across Canada, it is generalizable across hospital systems. “You can imagine the day that, if this were accepted, you could have this in the hospital computer system and it could be used by physicians to say, ‘This patient has a high risk of deteriorating—maybe we shouldn’t put them on the ward; maybe we should put them in intermediate care or a step-down unit.”
Although the study showed some of the risk factors leading to later ICU admission for patients with CAP, Dr. Russell said it is not as simple as developing a short list of risks to watch for. “It’s the subtleties around the edges,” he said. Even using logistic regression—which incorporates advanced statistics that a person cannot do at the bedside—the machine learning algorithms performed better by using the vast amount of a patient’s data on admission day.
What’s Next
Future studies may investigate how machine learning can be used to diagnose and treat bacterial pneumonia. “It’s a huge, very common healthcare issue, and there’s so much data on it,” Dr. Chen said. “So much about the care can be investigated and can be learned by looking at the data that we’ve already collected on patients.”
Dr. Russell is studying whether machine learning can predict whether a patient newly diagnosed with COVID-19 will have long COVID. He said, “There are probably many variables we don’t yet know that machine learning can help tease out through the type of algorithm that Dr. Chen identified in pneumonia.”